WHO WE ARE
The purpose of this website is not to provide medical advice. If you or a person requires medical care call 911 or the person’s medical care provider.
Many individuals living with a seizure disorder may feel unwelcome due to the prevalence of misconceptions surrounding seizures. At Seizure Free, we are dedicated to providing a supportive space for those with epilepsy and their caregivers. As the webmaster of this site, I have personally lived with epilepsy for over fifty-five years, offering a unique perspective that resonates with many others who share this journey. Our goal is to foster open and honest discussions, encouraging both the medical community and the wider public to address the myths and doubts that surround epilepsy. Join us on our blog page, where you can freely express yourself without fear of judgment. Together, let’s dismantle misconceptions and build a more understanding world.
What is Epilepsy?
We do not offer medical advice. For more concise information seek care of a licensed medical provider.
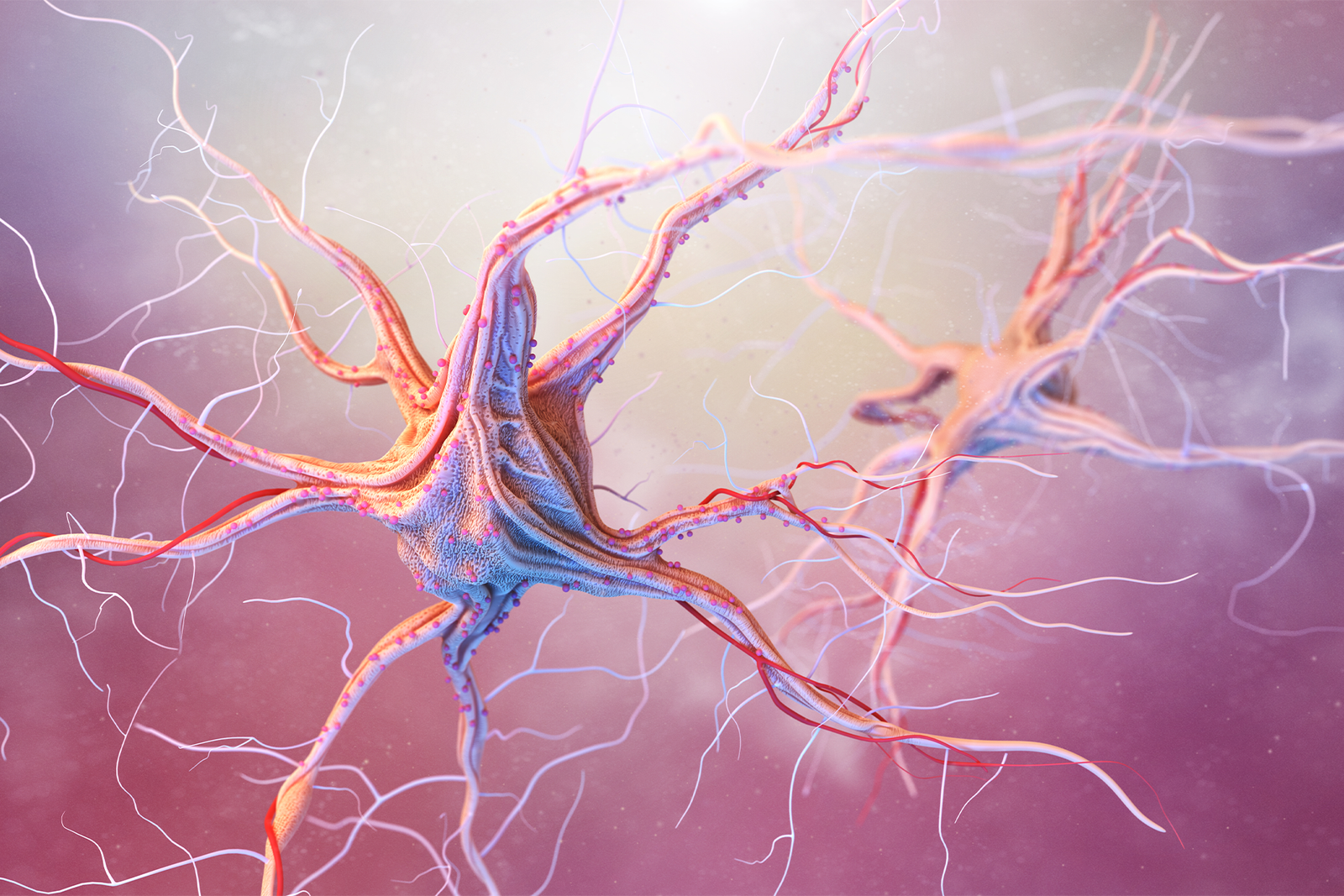
What is epilepsy?
Epilepsy is a neurological disorder characterized by recurrent seizures, which are sudden, uncontrollable electrical disturbances in the brain. These seizures can vary widely in their presentation, ranging from momentary lapses of awareness or muscle twitches to full-blown convulsions and loss of consciousness.
The exact cause of epilepsy is often unknown, although it can be attributed to various factors, including genetics, brain injuries, infections, prenatal injury, or developmental disorders. In some cases, epilepsy may be a result of a brain tumor or stroke.
Seizure Types
Seizures in epilepsy are classified into two main types:
- Focal seizures (partial seizures): These seizures originate in a specific area of the brain and can affect only one part of the body or cause unusual sensations or emotions. Focal seizures can be further divided into simple focal seizures (no loss of consciousness) and complex focal seizures (altered awareness or consciousness).
- Generalized seizures: These seizures involve both sides of the brain and can cause loss of consciousness and convulsions. Generalized seizures include absence seizures (brief loss of awareness), tonic-clonic seizures (previously known as grand mal seizures, involving muscle stiffening and jerking), atonic seizures (loss of muscle tone, causing sudden falls), and myoclonic seizures (sudden, brief jerks of the muscles).
How is epilepsy diagnosed?
Diagnosis of epilepsy typically involves a thorough medical history, neurological examination, and various tests such as electroencephalogram (EEG), MRI, and blood tests. Treatment usually includes antiepileptic medications to control or reduce the frequency and severity of seizures. In some cases, surgery or other interventions may be considered, especially if medications are ineffective or if there’s a specific underlying cause that can be addressed surgically.
Living with epilepsy involves managing the condition with medication, lifestyle modifications (such as getting enough sleep, avoiding triggers, and maintaining a healthy lifestyle), and regular medical follow-ups to monitor progress and adjust treatment as needed.
What are the causes of epilepsy?
Epilepsy can have various causes, and in many cases, the exact cause may not be fully understood. The development of epilepsy is often attributed to a combination of genetic, structural, metabolic, or developmental factors. Here are some common causes and risk factors associated with epilepsy:
Genetic Factors:
- Genetic predisposition plays a significant role in some cases of epilepsy. Certain genetic mutations or inherited tendencies can increase the likelihood of developing epilepsy. In some families, there may be a pattern of epilepsy or related neurological conditions, indicating a genetic influence.
- Brain Injuries and Trauma: Head injuries, traumatic brain injuries (TBIs), and brain trauma resulting from accidents, falls, sports injuries, or assaults can lead to epilepsy. Brain injuries may cause structural damage, inflammation, or disruptions in neuronal networks that contribute to seizure activity.
- Brain Tumors and Lesions: Benign or malignant brain tumors, as well as other types of brain lesions (such as cysts, scars, or vascular malformations), can trigger seizures if they affect areas of the brain involved in regulating electrical activity. Tumor growth or structural abnormalities can irritate brain tissue and lead to seizure development.
- Stroke and Vascular Disorders: Stroke, transient ischemic attacks (TIAs), aneurysms, arteriovenous malformations (AVMs), and other vascular disorders can disrupt blood flow to the brain, causing hypoxia (oxygen deprivation) and neuronal damage that may result in epilepsy.
- Infections and Encephalitis: Certain infections affecting the brain, such as meningitis, encephalitis, cerebral malaria, and brain abscesses, can lead to inflammation, scarring, and neuronal damage that predispose to epilepsy.
- Developmental Disorders: Some developmental conditions and neurological disorders, such as autism spectrum disorder (ASD), neurofibromatosis, tuberous sclerosis complex (TSC), and cerebral palsy, are associated with an increased risk of epilepsy due to abnormal brain development or structural anomalies.
- Metabolic and Electrolyte Imbalances: Metabolic disorders, electrolyte imbalances (e.g., sodium, calcium), and metabolic abnormalities (e.g., hypoglycemia, hyperglycemia, uremia) can disrupt neuronal function and trigger seizures.
- Neurological Diseases: Various neurological diseases and conditions, including Alzheimer’s disease, multiple sclerosis (MS), Parkinson’s disease, Creutzfeldt-Jakob disease, and Huntington’s disease, may be associated with epilepsy as a secondary symptom of underlying brain changes or neuronal dysfunction.
- Perinatal and Neonatal Factors: Complications during pregnancy, labor, or delivery, as well as prenatal exposure to toxins, infections, or maternal health conditions (e.g., pre-eclampsia), can increase the risk of epilepsy in infants and children.
- Drugs and Medications: Some medications, particularly certain antibiotics, antipsychotics, antidepressants, and antihistamines, may lower seizure thresholds and increase the risk of seizures in susceptible individuals.
- Alcohol and Substance Abuse: Excessive alcohol consumption, substance abuse (e.g., cocaine, amphetamines), and withdrawal from certain substances can trigger seizures, especially in individuals with a history of substance use disorders or alcohol dependence.
- Autoimmune and Inflammatory Conditions: Autoimmune disorders affecting the central nervous system (CNS), such as autoimmune encephalitis, systemic lupus erythematosus (SLE), and Hashimoto’s encephalopathy, can cause inflammation and neuronal dysfunction leading to seizures.
It’s important to note that epilepsy can develop at any age, and the underlying causes and risk factors can vary widely among individuals. In many cases, the cause of epilepsy may be multifactorial, involving a combination of genetic susceptibility, environmental factors, and neurological conditions. A thorough evaluation by healthcare providers, including neurological assessments, diagnostic tests (such as EEG, MRI), and medical history review, is necessary to determine the underlying cause and guide treatment strategies for epilepsy.
What is the difference between a seizure and epilepsy?
A seizure and epilepsy are related but distinct terms that refer to different aspects of neurological conditions involving abnormal electrical activity in the brain.
Seizure:
- A seizure is a sudden, temporary disruption in normal brain function caused by abnormal electrical activity.
- Seizures can manifest in various ways, including convulsions, muscle twitches, altered consciousness, unusual sensations, or behavioral changes.
- Seizures can be classified into different types based on their characteristics, such as focal (partial) seizures that originate in a specific area of the brain or generalized seizures that involve both sides of the brain.
- Seizures can occur as a result of various triggers, such as fever, head injuries, metabolic imbalances, medications, or neurological conditions.
- Not all seizures are due to epilepsy. Seizures can also occur as isolated events triggered by temporary factors, such as febrile seizures in children or seizures caused by acute medical conditions.
Epilepsy:
- Epilepsy is a chronic neurological disorder characterized by recurrent, unprovoked seizures.
- The diagnosis of epilepsy is made when a person has experienced at least two unprovoked seizures occurring more than 24 hours apart.
- Epilepsy can have various causes, including genetic factors, brain injuries, infections, structural abnormalities, metabolic disorders, and developmental conditions.
- Individuals with epilepsy may have different seizure types, frequency, severity, and response to treatment, depending on the underlying cause and specific characteristics of their condition.
- Epilepsy requires ongoing management and treatment, often involving antiepileptic medications, lifestyle modifications, and regular medical follow-ups to optimize seizure control and quality of life.
In summary, a seizure is a single, transient event of abnormal brain activity, while epilepsy is a chronic condition characterized by recurrent seizures. Seizures can occur in individuals with epilepsy as well as in people without epilepsy due to various triggers or temporary factors. Epilepsy specifically refers to the presence of recurrent, unprovoked seizures and requires medical evaluation, diagnosis, and management to address the underlying condition and reduce seizure frequency and impact.
What is the cure for epilepsy?
As of now, there is no definitive cure for epilepsy. However, the condition can often be effectively managed with appropriate treatment and lifestyle adjustments. The goal of epilepsy management is to reduce or eliminate seizures, improve quality of life, and minimize the impact of epilepsy on daily functioning. Here are some key components of epilepsy management:
- Antiepileptic Medications: The primary treatment for epilepsy involves using antiepileptic drugs (AEDs) or anticonvulsant medications to control seizures. These medications work by stabilizing neuronal activity in the brain and reducing the likelihood of abnormal electrical discharges that lead to seizures. The choice of medication depends on factors such as the type of seizures, the individual’s age and overall health, and potential side effects. It’s important for individuals with epilepsy to take medications as prescribed, adhere to dosage schedules, and regularly follow up with healthcare providers for monitoring and adjustments.
- Lifestyle Modifications: Certain lifestyle changes and modifications can help manage epilepsy and reduce seizure frequency. These may include:
- Maintaining regular sleep patterns and getting sufficient rest.
- Avoiding triggers that may precipitate seizures, such as sleep deprivation, stress, flashing lights, or specific foods.
- Managing stress through relaxation techniques, mindfulness, counseling, or support groups.
- Following a balanced diet, staying hydrated, and avoiding alcohol or recreational drugs that can lower seizure thresholds.
- Engaging in regular physical activity and maintaining overall health and well-being.
- Seizure Diaries and Monitoring: Keeping a seizure diary or journal to track seizure activity, potential triggers, medication adherence, and lifestyle factors can provide valuable information for healthcare providers. Regular monitoring of seizure frequency, severity, and response to treatment helps optimize management strategies and make necessary adjustments.
- Epilepsy Surgery: In cases of drug-resistant epilepsy or seizures that originate from a specific area of the brain, epilepsy surgery may be considered as a treatment option. Surgical interventions, such as temporal lobectomy, lesionectomy, hemispherectomy, or corpus callosotomy, aim to remove or disconnect the brain tissue responsible for seizures and reduce seizure activity.
- Neuromodulation Therapies: For individuals with refractory epilepsy who are not candidates for surgery or do not achieve adequate seizure control with medications, neuromodulation therapies may be recommended. These include techniques such as vagus nerve stimulation (VNS), responsive neurostimulation (RNS), deep brain stimulation (DBS), or transcranial magnetic stimulation (TMS) to modulate brain activity and reduce seizures.
- Ketogenic Diet and Alternative Therapies: Some individuals with epilepsy, especially children with certain epilepsy syndromes, may benefit from dietary therapies such as the ketogenic diet. Alternative therapies, including medical cannabis (cannabidiol/CBD) in specific formulations approved for epilepsy, may also be considered in certain cases under medical supervision.
It’s important to note that the effectiveness of epilepsy treatment varies among individuals, and management approaches may need to be personalized based on the individual’s unique characteristics, seizure types, response to treatment, and overall health. Regular communication with healthcare providers, adherence to treatment plans, lifestyle modifications, and ongoing monitoring are crucial for optimizing epilepsy management and improving quality of life for individuals living with epilepsy.

Support
Support

Educate Yourself
Your Subtitle Goes Here
Learn about epilepsy, including its causes, types of seizures, treatment options, and potential triggers. Understanding the condition can help you provide better support and respond appropriately during seizures or related challenges.
Encourage Medical Care
Your Subtitle Goes Here
Encourage the person with epilepsy to seek regular medical care, follow their healthcare provider’s recommendations, take medications as prescribed, and attend appointments for monitoring and treatment adjustments.
Promote Safety
Your Subtitle Goes Here
Create a safe environment by minimizing potential hazards and implementing safety measures. Remove sharp objects, cushion sharp corners, secure furniture, and avoid activities or situations that may increase the risk of falls or injuries during seizures.Create a safe environment by minimizing potential hazards and implementing safety measures. Remove sharp objects, cushion sharp corners, secure furniture, and avoid activities or situations that may increase the risk of falls or injuries during seizures.

Learn Seizure First Aid
Your Subtitle Goes Here
Familiarize yourself with seizure first aid techniques, such as staying calm, protecting the person from injury by cushioning their head and removing nearby objects, turning them on their side to maintain an open airway, and timing the seizure duration.
Encourage Open Communication
Your Subtitle Goes Here
Foster open and supportive communication with the person with epilepsy. Encourage them to share their experiences, concerns, and needs related to their condition, treatment, and daily life.

Respect Privacy and Dignity
Your Subtitle Goes Here
Respect the person’s privacy and dignity regarding their epilepsy. Avoid making assumptions, judgments, or stigmatizing comments. Offer support and understanding without undermining their autonomy or self-esteem.

Be Flexible and Understanding
Your Subtitle Goes Here
Epilepsy can be unpredictable, and seizure activity may vary. Be flexible and understanding if plans need to change due to seizures or related challenges. Offer patience, empathy, and reassurance during difficult times.
Provide Practical Support
Your Subtitle Goes Here
Offer practical assistance with daily tasks, transportation to medical appointments, medication reminders, and access to resources such as support groups, educational materials, and community services.

Encourage Healthy Lifestayle Choices
Your Subtitle Goes Here
Promote a healthy lifestyle that includes regular sleep patterns, stress management techniques, balanced nutrition, regular physical activity, and avoidance of seizure triggers such as alcohol or drug use.

Be An Advocate
Your Subtitle Goes Here
Advocate for the person with epilepsy’s rights, needs, and access to healthcare, education, employment, and community participation. Raise awareness, combat stigma, and promote inclusivity and acceptance.

Offer Emotional Support
Your Subtitle Goes Here
Be a supportive listener, offer encouragement, validate feelings, and provide emotional support during challenging times. Encourage the person to seek counseling or mental health services if needed.v
Prepare For Emergencies
Your Subtitle Goes Here
Be prepared for potential emergencies by having an emergency action plan, knowing who to contact in case of seizures or medical emergencies, and being familiar with emergency medications or devices if prescribed.v
Congressional Record – Senate S733
Senator Sherrod Brown makes appeal to Congress So if we repeal the Affordable Care Act, somebody has to explain to those 700,000 people why they no longer have insurance, why those 100,000 young people are getting dropped from coverage; those families like the woman’s...
Meet The People Whose Lives Have Been Transformed By Medicaid Expansion
Charles McClinon, a 50-year-old Ohio resident who lives with epilepsy, told ThinkProgress, “The peace of mind is worth more than anything. I could be a millionaire, but if I don’t have peace of mind, what good is it? And that’s one thing this type of insurance is good...
Obamacare Brings Dramatic Changes for Uninsured, Hospitals, Insurers
Randy Tucker, Dayton Daily News, Ohio Sept. 28--The impact the Affordable Care Act has had on the previously uninsured and low and middle income families cannot be understated as millions of Americans and tens of thousands of Ohioans have gained access to health...